Recently, a message from a clinic in Singapore advising patients that a Pap smear test could cause them to ‘lose their virginity’, has sparked considerable public discussion and confusion. This claim is a harmful misunderstanding about a vital women’s health screening.
At Doctor Anywhere, we believe in clear, factual medical communication. It’s vital to understand exactly what a Pap smear is, what it isn’t, and why it’s a nationally recommended, life-saving procedure.
What Exactly is a Pap Smear?
A Pap smear, also known as a Pap test or cervical screening test, is a quick and essential procedure designed to detect abnormal cells in the cervix. The cervix is the lower part of the uterus that connects to the vagina. These abnormal cells, if left untreated, could potentially develop into cervical cancer.
During the test, a small instrument is gently inserted into the vagina to help the doctor see the cervix clearly. A small spatula is then used to collect a sample of cells from the cervical surface and the procedure usually takes only a few minutes. These cells are then sent to a laboratory for analysis and testing.
Dispelling the Virginity Myth
The idea that a Pap smear causes a woman to “lose her virginity” is a deeply rooted and harmful misconception. Medically, a Pap smear is a diagnostic procedure; it has no bearing on a person’s sexual experience or virginity.
The misunderstanding often stems from a misconception about the hymen. The hymen is a thin piece of tissue that partially covers or surrounds the vaginal opening. It is not a sealed barrier and can vary greatly in size and shape from person to person. Crucially, the hymen is not a reliable indicator of virginity, and it can stretch or tear due to various non-sexual activities, such as:
- Inserting a tampon
- Strenuous exercise like cycling, gymnastics, or horseback riding
- Other physical activities or even medical examinations
It is vital to understand that a Pap smear is a medical procedure to collect cells for cervical cancer screening; it does not, in any medical or social sense, cause a woman to ‘lose her virginity’. Medical professionals are trained to perform this important and sometimes life-saving test with utmost care and respect for patient comfort and privacy. No woman should avoid this crucial screening due to misinformation or fear.
A Comprehensive Approach to Cervical Cancer Prevention
Cervical cancer is largely preventable, primarily because it is caused by persistent infection with certain types of Human Papillomavirus (HPV). Protecting yourself involves a two-pronged approach:
- HPV Vaccination: The HPV vaccine works by preventing infection by the high-risk HPV strains that cause the vast majority of cervical cancers. It is recommended for both boys and girls, and even adults up to age 45, ideally before sexual activity begins, but it can still offer protection against strains not yet encountered.
- Cervical Screening (Pap or HPV Test): While vaccination prevents the initial infection, screening detects any pre-cancerous cellular changes in the cervix that HPV might have caused. This allows for early intervention and treatment before cancer can develop. Singapore’s national recommendations suggest that sexually active women from the age of 25 should undergo regular cervical screening, typically every three years.
Both HPV vaccination and regular cervical screening are crucial and complementary strategies in the fight against cervical cancer.
New CERVICAL Screening Methods
Statistics show that about 70% of women in Asia avoid Pap smears, which is why new less invasive screening methods are increasingly being explored. These innovations include HPV self-sampling, a convenient method where women can collect their own sample privately at home (trialled by the Singapore Cancer Society and its partners, Alliance for Active Action Against HPV (A4HPV)). Another exciting development is sanitary pad testing, pioneered by Hong Kong scientist Dr. Pui-wah Choi, which aims to transform screening by testing period blood on a pad.
While these innovations offer incredible possibilities, they are currently in trial or development.
For now, in-clinic Pap smears and HPV tests remain the primary recommended and most widely available methods for cervical cancer screening.
Don’t Delay Your Screening
Your health should always come first. Dispelling misinformation and understanding the facts about Pap smears empowers you to make informed decisions about your well-being. Regular cervical screening, alongside HPV vaccination, are simple, effective steps you can take to protect yourself against cervical cancer.
If you have concerns or are due for a screening, please speak to a trusted doctor.
Need to book a cervical screening or simply discuss your women’s health concerns?
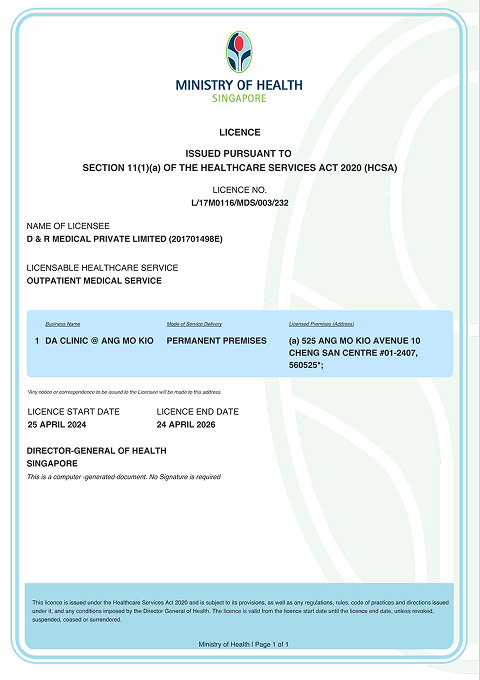
📲 Book a teleconsult with a Doctor Anywhere GP or visit a DA clinic today.